Glioblastoma
The Common Vein Copyright 2010
Definition
A glioblastoma is the most common subcategory of astrocytoma, which is a subtype of glioma, or tumor arising from glial cells. This most aggressive and most common of the astrocytoma is characterized pathologically and distinguished from other less aggressive astrocytomas by the presence of necrosis and vascular or endothelial proliferation.
The etiology of most glioblastomas is usually unknown. There has been a familial link in a minority of cases as well as associations with known genetic syndromes such as neurofibromatosis or Turcot syndrome. Glioblastoma may also arise secondarily from within a preexisting lower grade glioma. These aggressive tumors infiltrate large areas of otherwise normal brain making complete resection impossible and due to their aggressive behavior they most often lead to death shortly after presentation.
These tumors tend to arise within the cerebral hemispheres, presenting with a range of symptoms depending on their location. Frequently, affected patients present with headache or motor weakness. Other common presenting symptoms include nausea and vomiting due to the mass effect of the tumor or seizures.
Diagnosis is suspected clinically and confirmed by imaging in conjunction with pathologic analysis. Given the heterogeneity of this particular tumor, however, a sample or biopsy may not fully characterize this lesion.
Glioblastomas may be imaged by both CT and MRI. On CT they appear as irregular hypoattenuating mass lesions centered in the white matter with significant mass effect. On MRI, these tumors are T1 hypointense and heterogeneous but predominantly hyperintense on T2 with generally a thick rind of enhancement. Glioblastomas may cross the white matter tracts of the corpus callosum in a pattern described as a butterfly glioma.
Treatment of glioblastoma includes resection followed by radiation and chemotherapy however the prognosis remains poor with mean length of survival of approximately 15 months after diagnosis
|
Glioblastoma of the Splenium |
|
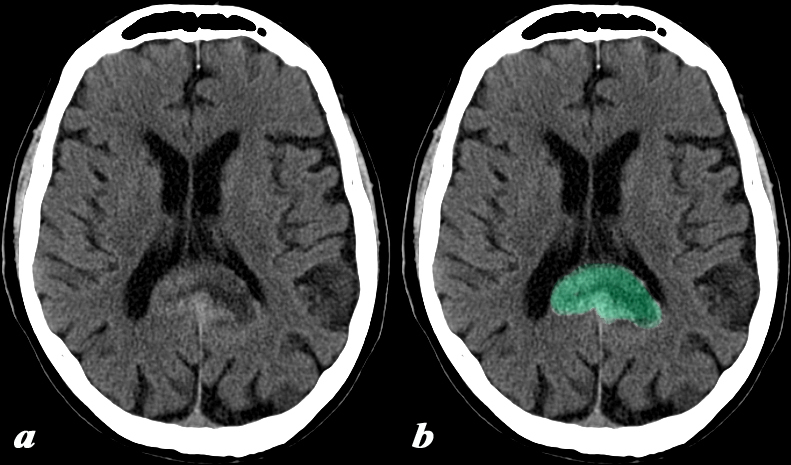
This 74 year old male presented with memory impairment and confusion. CT: (a,b) This head CT obtained without contrast demonstrates irregular enlargement of the splenium of the corpus callosum which has abnormal decreased central and increased peripheral density (green b), and crosses the midline. These findings are consistent with a diagnosis of glioblastoma multiforme. Included in the differential diagnosis for lesions crossing the midline is primary lymphoma of the brain Image Courtesy Elisa Flower MD and Asim Mian MD 97644c.8 |
|
T1 T2 and FLAIR |
|
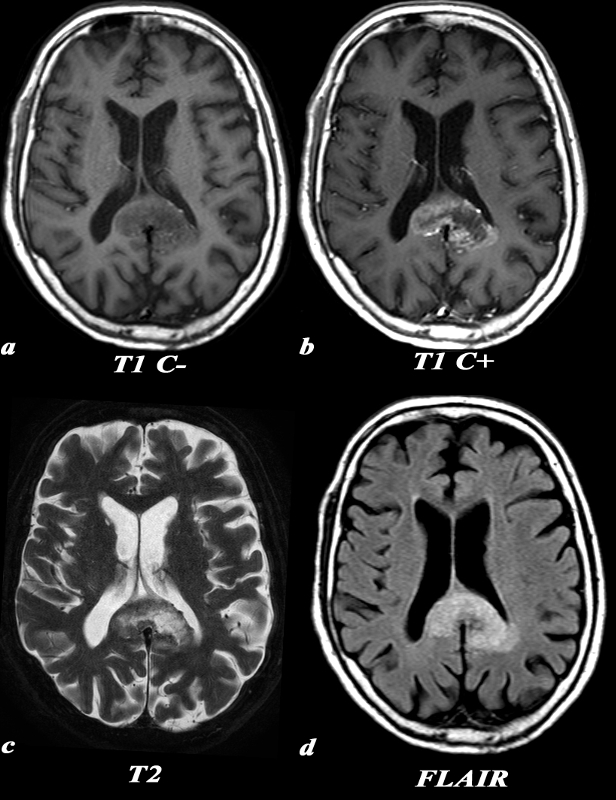
This 74 year old male presented with memory impairment and confusion. A previously performed head CT had shown a space occupying lesion in the splenium of the corpus callosum (above). MRI: (a,b,c,d) T1 weighted axial images before contrast (a) demonstrates a low signal in the enlarged splenium of the corpus callosum. The post contrast T1 weighted image (b) in the axial plane demonstrates the peripheral and irregular enhancement of the mass. This configuration is classic and often called a “butterfly” glioma. Remember that due to the infiltrative nature of the mass, the extent of actual tumor involvement is larger than what is demonstrated by imaging on the post contrast images. This lesion which is hyperintense on T2 (c), enlarges the splenium, crosses the midline and involves the medial aspect of the left parietal lobe. Similar findings are identified on the FLAIR image. The extension into the parietal lobe is best seen on the FLAIR image These findings are consistent with a diagnosis of glioblastoma multiforme. Included in the differential diagnosis for lesions crossing the midline is primary lymphoma of the brain Image Courtesy Elisa Flower MD and Asim Mian MD 97647c01.8 |
|
Glioblastoma of the Spelnium of the Corpus Callosum |
|
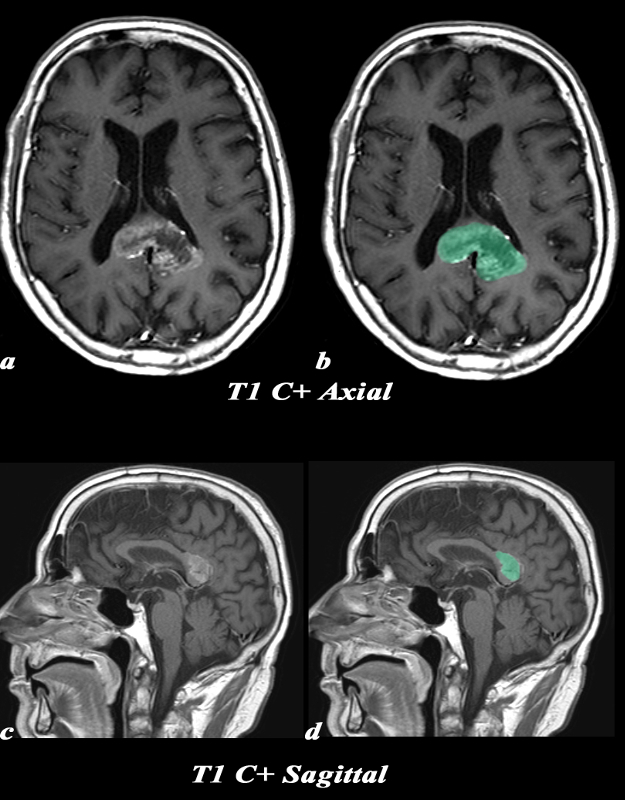
This 74 year old male presented with memory impairment and confusion. A previously performed head CT had shown a space occupying lesion in the splenium of the corpus callosum. MRI: (a,b,c,d) T1 weighted axial images after contrast (a) demonstrates peripheral and irregular enhancement of the mass overlaid in green in b,. This configuration is classic and often called a “butterfly” glioma. Remember that due to the infiltrative nature of the mass, the extent of actual tumor involvement is larger than what is demonstrated by imaging on the post contrast images. The sagittal image(c,d) is a T1 weighted sequence following gadolinium and shows that the lesion is originating from the splenium of the corpus callosum. These findings are consistent with a diagnosis of glioblastoma multiforme. Included in the differential diagnosis for lesions crossing the midline is primary lymphoma of the brain Image Courtesy Elisa Flower MD and Asim Mian MD 97647c02.8 |
|
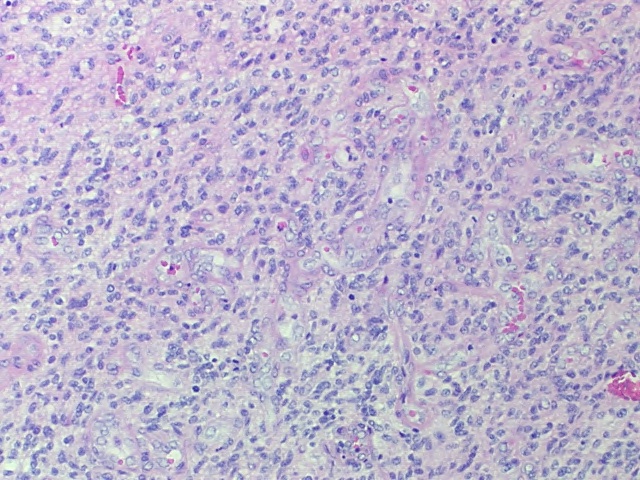
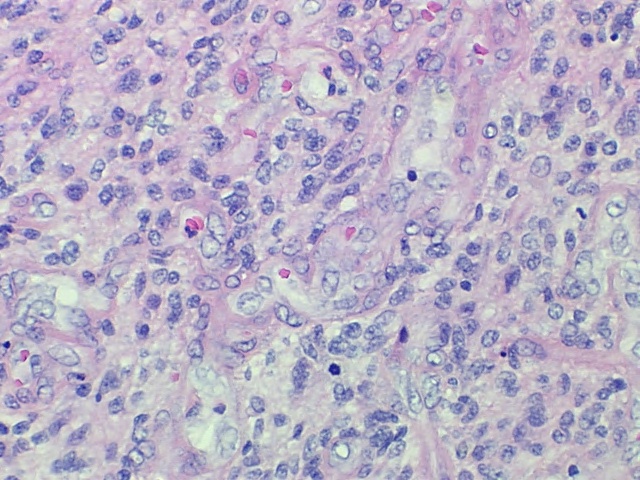
Low Power H&E High density of hyperchromatic, pleomorphic cells.
High Power H&E High density of hyperchromatic, pleomorphic cells. Multiple mitoses can be identified as the dark cell nuclei
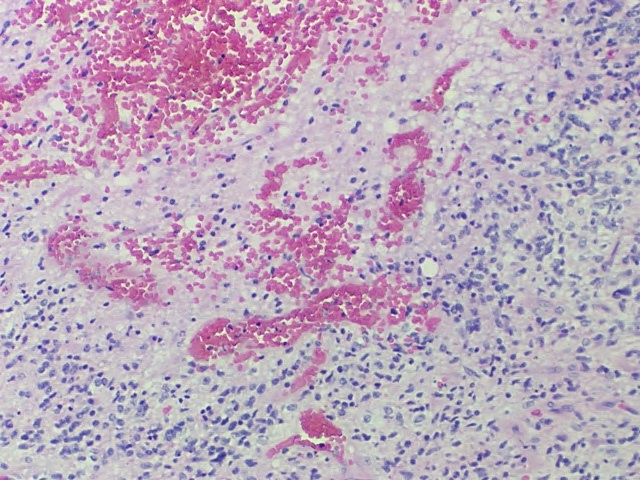
Vascular Endothelial Prolifereation Glioblastoma |
|
The diagnosis of glioblastoma can be made on these low and high power polymicrographs alone, without the need for additional immunohistochemical staining. There is a high density of hyperchromatic, pleomorphic cells. Multiple mitoses can be identified as the dark cell nuclei, better seen on the high power image. Additionally, there is evidence of vascular endothelial proliferation. Image Courtesy of Cheryl Spencer, M.A. and Ivana Delalle, MD, PhD Department of Pathology Boston University School of Medicine 98499500/501 (S07-17336) |