Intracerebral Hemorrhage
The Common Vein Copyright 2010
Introduction
Intracerebral hemorrhage occurs when an intracerebral blood vessel is ruptured. This rupture can be caused by trauma, stroke, spontaneous rupture (frequently aneurysms), neoplasms, vasculitides.. It results in accumulation of blood, which arises in the brain parenchyma itself and may extend into the subarachnoid space.
Structurally, the extravasation of blood may compress the brain parenchyma. It is therefore characterized by the presence of clotted blood and surrounding edema. Subarachnoid extension of the hemorrhage, commonly extends from rupture of aneurysms or arteriovenous malformations.
Clinically, patients have loss of consciousness, initial or later in the course as bleeding proceeds, headaches, seizures and focal symptoms.
Diagnosis is made by CT or MRI.
Treatment is symptomatic, but in some instances decompressesion by craniotomy prevents the dreaded complication of coning.
Acute
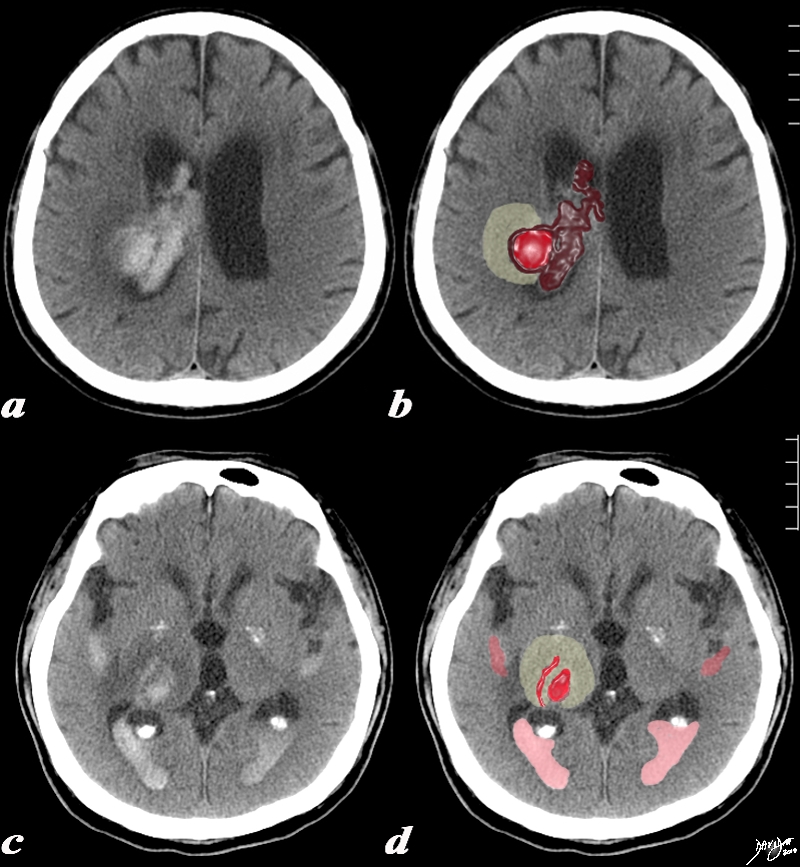
Acute Right Thalamic Hemorrhage |
|
The CT is from a 77year old male with acute neurological deficit The epicenter of the disease is an acute hemorrhage in the right thalamus, bright red in (b,d) with extension of the clot into the ventricle (maroon). There is non clotted blood lying dependently in the occipital horns (dense on c) presenting as a CSF-blood level (light pink on black CSF) in (d). The hemorrhage is surrounded by a rim of edema (light yellow) as seen in b and d. Courtesy Ashley Davidoff MD Copyright 2010 All rights reserved 90461c03.8s |
|
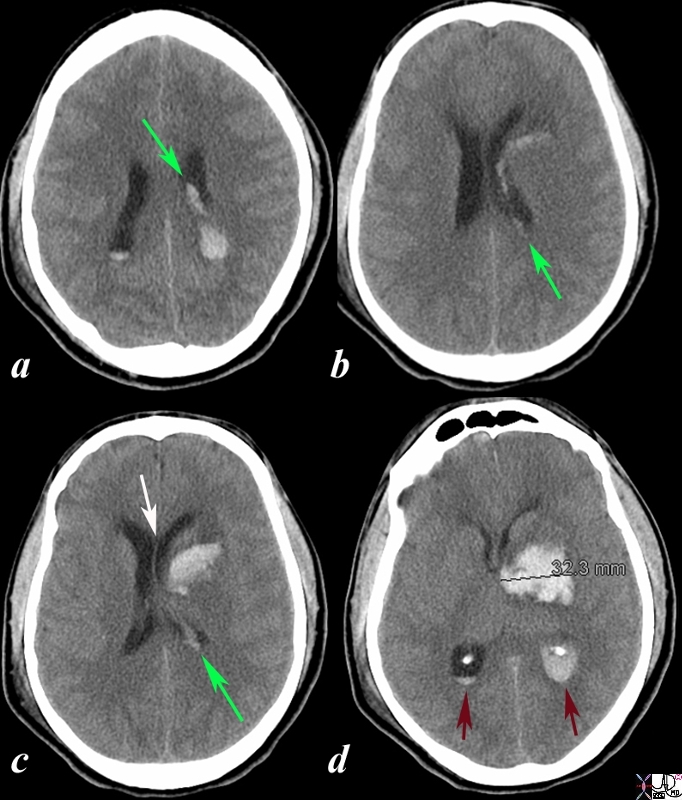
Acute Hemorrhagic Stroke of the Basal Ganglia Hemorrhage from the Perforators Rupture into the Choroid Plexus |
|
The CT is from a 33year old male with an acute left basal ganglial hemorrhagic stroke. The CT shows a hyperdense accumulation of hemorrhage(d) complicated by extension or rupture of the hemorrhage into the ipsilateral choroid plexus (green arrows a,b,c) and hemorrhage into the ventricles with blood lying dependently in the occipital horns (maroon arrows in c) and midline shift with septum pellucidum (white arrow of the eyes (lenses overlaid in d) mass effect on the left frontal horn (d) and midline shift exemplified by the shift of the septum pellucidum (white arrow c). Image Courtesy Ashley Davidoff MD Copyright 2010 98551cL.8s |
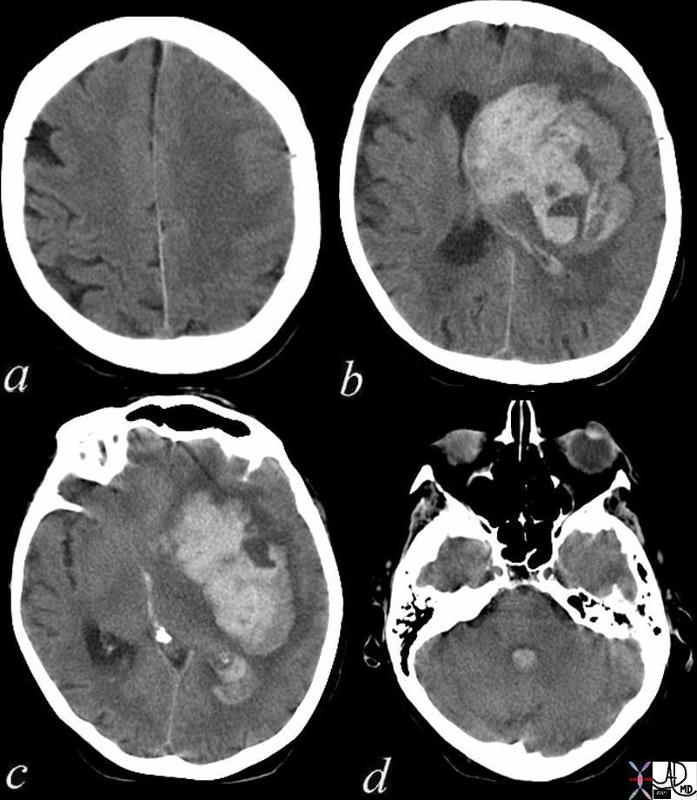
Acute Cerebral Hemorrhage with Mass Effect and Rupture into the Ventricles |
| This CT shows an acute hemorrhagic event originating in the frontoparietal region of the left cerebral hemisphere causing significant mass effect by compressing and displacing the ipsilateral lateral ventricle with significant midline shift.
The hemorrhage has ruptured into the ipsilateral lateral ventricle and blood can be seen within the choroid plexus (b) in the posterior horn (c) as well as the 4th ventricle (d). The ipsilateral edema has caused loss of the gray white matter interface in the left parietal lobe Courtesy Ashley Davidoff MD Copyright 2010 72143c01 |
Acute MRI
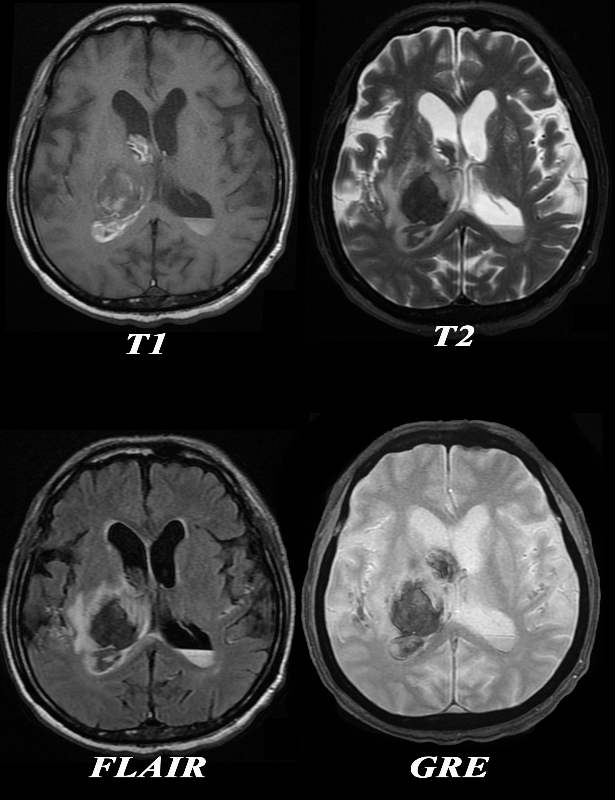
Acute Thalamic Hemorrhage MRI |
|
The MRI is from a 77year old male with acute neurological deficit The epicenter of the disease is a hemorrhage in the right thalamus. The T1 weighted image (upper left) shows mostly hypointense signal indicating the presence of deoxyhemoglobin. On the T2 weighted image the signal of the hematoma is also mostly hypointense confirming the hyperacute nature of the hematoma, surrounded by a ring of increased signal reflecting edema. There is a layering effect of blood in the posterior horn on the left The presence of deoxyhemoglobin dates the hemorrhage between minutes to hours The FLAIR image (c) shows the hyperacute hematoma as hypointense and the surrounding edema as hyperintense. The GRE image fails to reveal hemosiderin deposit in the periphery making chronic hemorrhage unlikely. The diagnosis of hyperacute intracerebral hemorrhage (minutes to hours) is therefore made by the presence of deoxyhemoglobin hypo/isointensity on the T1 weighted images and the hypointensity on T2 weighted. The suurounding edema is best seen on the T2 and FLAIR images. The extension into the ventricles is apparent on all sequences. Courtesy Ashley Davidoff MD Copyright 2010 All rights reserved 90484c04.8 |
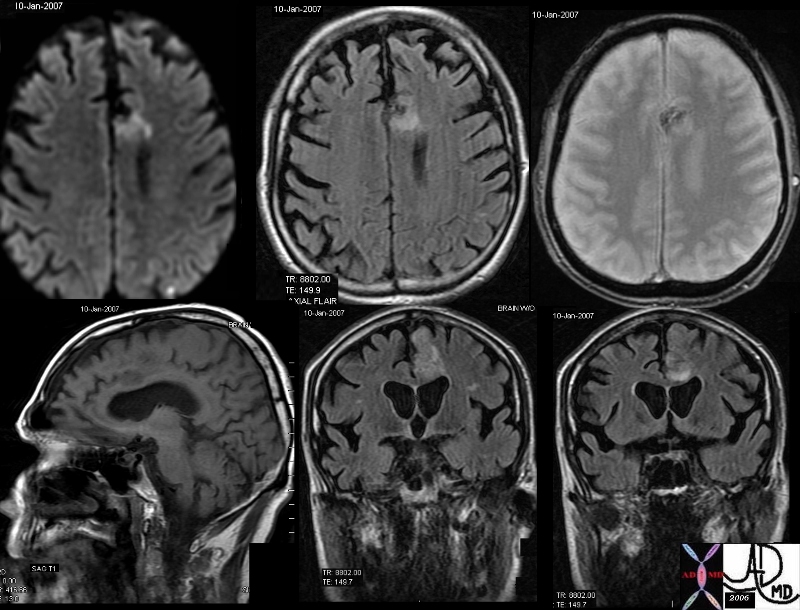
Acute Frontal Lobe hemorrhagic Infarction |
| The MRI in various projections confirms the presence of an acute hemorrhagic infarct in the left paracentral frontal territory. The diffusion images (top left), show a hyperintense focus in the left frontal lobe, which is hyperintense on the axial FLAIR image (middle top), hypointense and granular on the GRE (top right), hypointense on the sagittal T1 (bottom left) and seen as hyperintense on the last two STIR coronal images. These findings are consistent with an acute hemorrhagic focus which and was thought to be embolic in origin due to other noted foci. brain frontal lobe fx hyperintense focus diffusion images fx hyperintense T2 weighted STIR fx dark GRE fx dark T1 dx hemorrhagic infarction hemorrhage acute bleed dx acute hemorrhagic emboli MRI
Courtesy Ashley Davidoff MD copyright 2010 46098c01.800 |