Metastases
The Common Vein Copyright 2010
Deinition
Intracranial metastases are characterized as a secondary brain neoplasm. They are the most common infratentorial mass in adults. Metastatic lesions tend to be round masses which occur at the gray- white matter junction, where the blood vessels become quite small in caliber. They can be either solitarty or multiple, each found fifty percent of the time. Primary breast, lung, melanoma, renal and thyroid cancers have a high propensity for parenchymal CNS metastases. Certain primary tumors can also metastasize to the dura, including lung, breast, prostate, and melanoma
Many of these lesions have a propensity to bleed, resulting in hemorrhagic lesions. This is seen more commonly in renal, melanoma, thyroid and breast carcinomas.
Clinical presentation, as with most other brain masses, depends on location.
Diagnosis is suggested by clinical history of primary malignancy and imaging findings, however primary may not be known at time of initial radiologic workup.
Imaging of intracranial metastases includes primarily CT and MRI. The imaging characteristics of metastases depend on the type of primary lesion. Most metastases are hypoattenuating on CT, however some may demonstrate regions of high density from calcification or hemorrhage. On MRI, most metastases are T2 hyperintense to gray matter and T1 hypointense masses with a variable amount of surrounding vasogenic edema. When located at the gray white matter junction, they demonstrate significant vasogenic edema, as opposed to cortical metastasis which may simply appear as regions of enhancement without significant surrounding edema. Occasionally, their T1 signal may be high due to hemorrhage. Nearly all metastases enhance, but the pattern is quite variable and may be uniform, nodular or peripheral for example. Dural based masses appear as focal masses or regions of dural thickening which classically enhance.
Treatment of brain metastasis depends on many factors, including the overall condition of the patient, location and number of metastatic lesions and presence of mass effect. Surgical resection is possible if the lesion is in a noneloquent portion of the brain. Radiosurgery is another option as is chemotherapy.
Metastasis
The Common Vein Copyright 2010
Definition
Cancer can disseminate and colonization distant sites of the body, forming secondary tumors, called metastases, and the brain is a potential site. This results in a mass causing increased intracranial pressure, with possible focal or diffuse disorder of cerebral function.
Structurally, metastases are round well-demarcated lesions that are usually located at the junction of gray and white matter. They are surrounded by edema, because the tumor vessels are usually leaky, and at times, they can originate a hemorrhage. They can also be localized in the skull and the meninges.
Spread of the primary tumor to the brain occurs through blood circulation, mostly from the arterial circulation, although it can also occur through the Batson venous plexus. Most often, lung tumors are the ones to metastasize to the brain, since arterial blood passes through the lungs before going to the brain, thus “filtering” most metastatic tumor cells, though this is not always necessarily true. Melanomas and breast neoplasias are other tumors that often metastasize to the brain.
Patients have vague complains of headache, lethargy, nausea and vomiting. As in intracranial masses, there can be focal and diffuse symptoms, such as hemiparesis, cranial nerve palsies, hemisensory deficits, aphasia, visual field deficits, seizures, ataxia.
MRI, with contrast enhancement, is preferred to CT modalities, since it allows detection of more lesions than CT., being more sensitive and specific. Lesions with vasogenic edema and mass effect will be seen in both. They are isointense in T1 and hyperintense in T2 and FLAIR. Contrast induces a irregular ring enhancement pattern. On CT, density is variable and non-diagnostic, but contrast can show a similar enhancement pattern.
Typically, patients with brain metastasis carry a poor prognosis. At best, they often die within 2 years, despite resection, chemotherapy and radiotherapy.
|
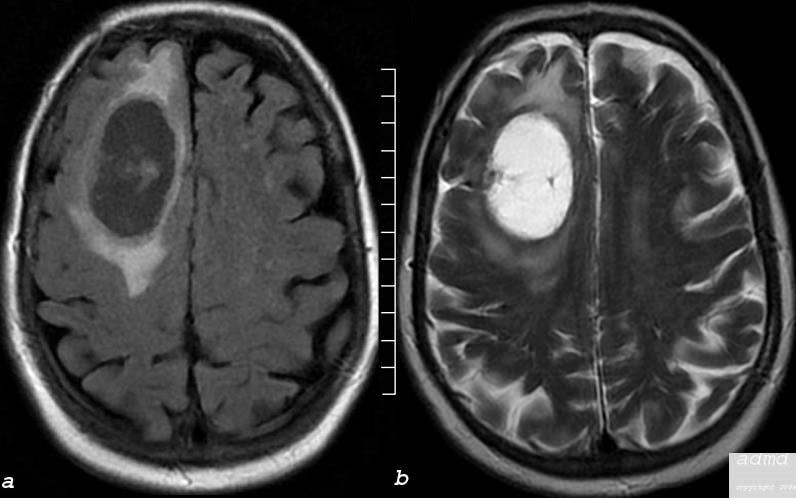
Cystic Metastasis FLAIR and T2 Weighted Image |
|
The MRI performed in the axial plane shows a large mass in the right frontal region and the anterior half of the centrum semiovale. Image (a) is an axial image through the vertex of the brain using FLAIR technique showing mostly a cystic type lesion with some internal thick sepatation with surrounding vasogenic edema. Minimal mass effect on the midline is perceived. Image (b) is an axial T2 weighted sequence showing a cystic matrix and surrounding edema The lesion was shown to be a cavitating squamous cell metastasis brain frontal lobe mass cystic moderate surrounding edema consistent with squamous cell carcinoma metastasis edema involves the anterior half of the right centrum semiovale Courtesy Ashley Davidoff MD Copyright 2010 75408c03 |
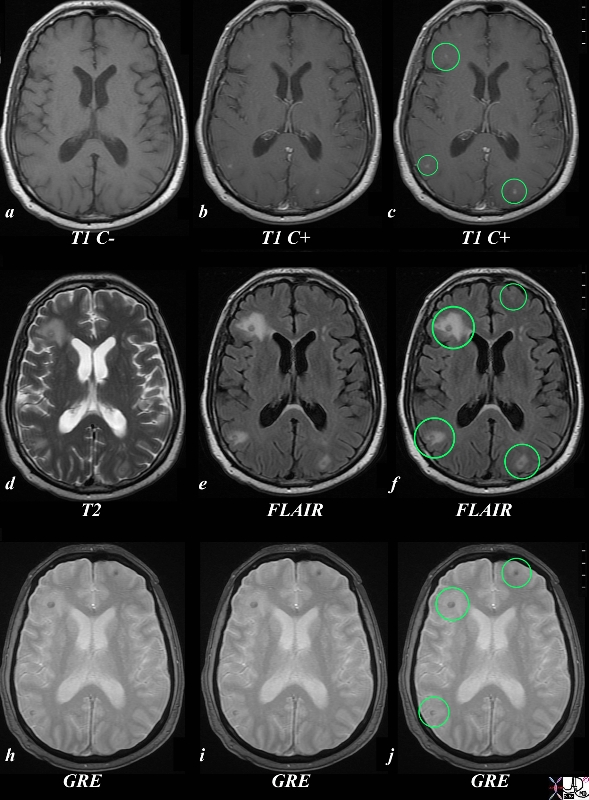
Small Metastases from Prostate CArcinoma Value of Multiplae Sequences for Characterization |
|
The MRI of the brain in a patient with prostate carcinoma shows evidence of metastatic carcinoma to the brain. The T1 weighted image without contrast (a) shows a barely visible target lesion in the right frontal lobe with central hypointensity and a narrow rim of hyperintensity. The gadolinium enhanced images (b and c) show punctate areas of enhancement in the right frontal, right posterior parietal and left occipital regions (ringed in green). The T2 weighted image (d) reveals the vasogenic edema around the frontal metastasis, but the FLAIR images show the vasogenic edema around the two other lesions described by greater sensitivity to the vasogenic edema.(green rings) but also suggests a vague left frontal lesion (green ring f) The GRE images show susceptibility in 3/ 4 lesions (ringed suggests the presence of hemosiderin. These findings are consistent with multifocal metastases to the brain likely from the prostate carcinoma, and also suggest the presence of chronic punctate hemorrhages. Image Courtesy Ashley Davidoff MD Copyright 2010 89546c.8s |